Sjögren-Larsson Syndrome: A Patient's Perspective: A Clinical Perspective
All images are copyrighted by FIRST or used with proper consent. They may not be downloaded or re-used for any purpose.
What is Sjögren-Larsson Syndrome (SLS)?
SLS is a form of ichthyosis associated with other symptoms involving the brain and nervous system. SLS is caused by alterations (mutations) in the gene for an enzyme (fatty aldehyde dehydrogenase) that is necessary for metabolism of certain unusual fats (lipids/ called fatty aldehyde and fatty alcohol. It is thought that the symptoms of SLS are a direct result of accumulation of these unusual lipids in the body or possibly due to an inability to produce other lipid metabolites that are normally made by the enzyme.
What are the Signs & Symptoms?
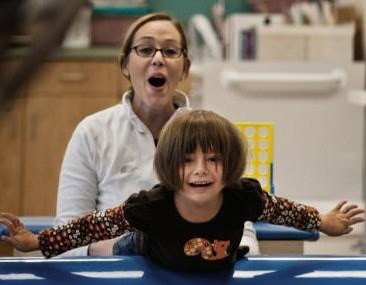
Patients are usually born with evidence of ichthyosis, but they soon show developmental delay in the first year or two of life, especially in their motor abilities such as sitting up or walking. Speech is often delayed or indistinct, and retinal (eye) abnormalities are frequently present. Some children have seizures. Unlike most other forms of ichthyosis, many SLS children are bothered by severe itchiness of their skin.
How is it diagnosed?
SLS is diagnosed by testing for the deficient enzyme in cultured skin fibroblasts grown from a skin biopsy or by finding mutations in the SLS gene, which can be done on a DNA sample from blood. Only about 50% of children with the typical symptoms of SLS (ichthyosis, developmental delay and spasticity) turn out to have the disease when tested. The rest have other forms of ichthyosis-some with unknown diseases. In general, the skin biopsy is not very helpful in diagnosing SLS, whereas enzyme testing and DNA analysis are definitive.
Doctors frequently use genetic testing to help define which ichthyosis a person actually has. This may help them to treat and manage the patient. Another reason to have a genetic test is if you or a family member wants to have children. Genetic testing, which would ideally be performed first on the person with ichthyosis, is often helpful in determining a person's, and their relative's, chances to have a baby with ichthyosis. Genetic testing may be recommended if the inheritance pattern is unclear or if you or a family member is interested in reproductive options such as genetic diagnosis before implantation or prenatal diagnosis.
Results of genetic tests, even when they identify a specific mutation, can rarely tell how mild or how severe a condition will be in any particular individual. There may be a general presentation in a family or consistent findings for a particular diagnosis, but it's important to know that every individual is different. The result of a genetic test may be "negative," meaning no mutation was identified. This may help the doctor exclude certain diagnoses, although sometimes it can be unsatisfying to the patient. "Inconclusive" results occur occasionally, and this reflects the limitation in our knowledge and techniques for doing the test. But we can be optimistic about understanding more in the future, as science moves quickly and new discoveries are being made all the time. You can participate in research studies and also receive genetic testing through the National Ichthyosis Registry at Yale University or for more information about genetic tests performed you can visit GeneDx, www.genedx.com.
What is the treatment for SLS?
There is no really effective treatment for SLS. The skin can respond to the usual topical lotions and keratolytic agents, hut the neurologic symptoms have no specific therapy. Walking ability can often benefit from surgical procedures that improve the spasticity. The itchiness of some patients may respond to a drug called zileuton (Zyflo), but this drug is not approved by the FDA for use in children.
Currently, my child has mobility in his arms and legs; what is the likelihood of future neurological or motor inability?
This is difficult to predict for any one patient. Most children with SLS have spastic diplegia (resembles cerebral palsy) that results in impaired walking. Some children never walk, but most do walk with assistance (crutches, walkers, etc). Others with mild spasticity are able to walk independently.
Should my child see an ophthalmologist to detect early retinal abnormalities?
In some SLS children, an ophthalmologist can detect abnormalities in the retina (the part of the eye that detects vision) called "glistening white dots," which are relatively specific for this disease. The retinal findings of SLS are usually seen after about 1-2 years of age. Blindness does not occur in SLS, but slight visual impairment requiring glasses is often present. More frequent is photophobia
My baby is six months old. Should she be on any special fat-modified diet to help with her disease?
Our experience is that the diet has no consistent effect on SLS. However, there are several reports in the medical literature of variable improvement of the skin using diets supplemented with medium-chain fatty acids, but we saw no effect of this when we studied 5 children. Nor is it clear whether special diets that limit consumption of the lipids that cannot be metabolized in SLS children are beneficial. Clearly, more research is needed on the therapeutic effects of dietary modification in this disease.
My husband and I are thinking about having additional children. What is the risk that my future children will be affected with SLS?
There is a 25% chance that future children will be affected with SLS. This risk is identical for each future pregnancy and is not reduced because you already have one SLS child. Prenatal diagnosis can be done to detect an affected fetus using DNA or enzyme tests done in the first or second trimester.
Download a PDF version of this information
 |
This column has been answered by Dr. William Rizzo. Dr. Rizzo is a member of FIRST's Medical and Scientific Advisory Board. He practices at the Department of Pediatrics at the University of Nebraska Medical Center in Omaha, Nebraska. |
Why are the images hidden by default? Can I change this?


All images are copyrighted by FIRST or used with proper consent. They may not be downloaded or re-used for any purpose.
| Other Names: | None |
| OMIM: | 270200 |
| Inheritance: | autosomal recessive |
| Incidence: | Not available at this time |
| Key Findings: |
|
| Associated Findings: |
|
Additional Resources:
- Clinicians seeking to confirm a diagnosis should visit FIRST's TeleIchthyosis site to submit a case to experts in ichthyosis. »
- Learn more about FIRST's Support Services - connecting affected individuals and families with each other. Or call the FIRST office at 800-545-3286. »
- Information about current clinical trials and research studies can be found here.